Should I See a Chiropractor for a Bulging or Herniated Disc?
Many people use the terms slipped disc, bulging disc, and herniated disc interchangeably. They are related, but they are not all the same thing. Understanding the difference helps you make smarter treatment choices and avoid unnecessary stress or fear when pain strikes.
Is a Slipped Disc the Same as a Bulging Disc?
In Chiropractic practices, slipped disc is a non-medical term patients often use to describe a disc that has been injured and moved past its usual boundary and is causing symptoms. This is not a diagnosis.
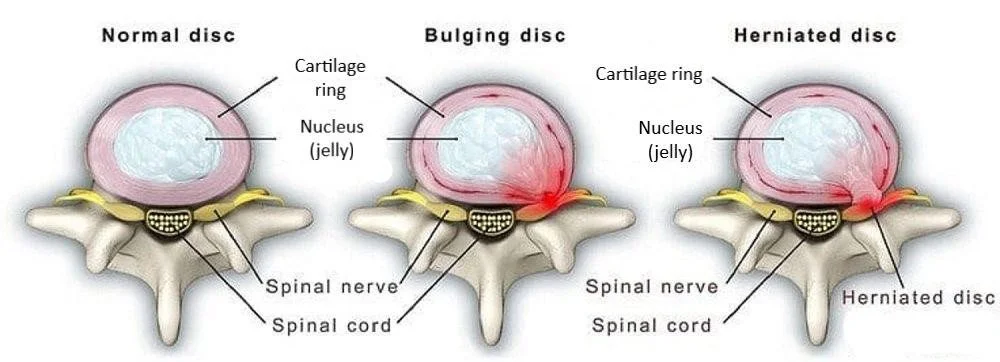
A disc bulge means the inner part of the disc is pushing outward but still contained within the outer ring (annulus fibrosus). The shape changes, and pressure can increase, but nothing has ruptured. This is also often known as a disc tear because some of the fibres have lost their integrity.
A true herniation means the inner material (nucleus pulposus) has broken through a tear in the annulus, creating a higher chance of nerve irritation, and is very serious.
Take-home message:
A slipped disc may refer to a bulge or a herniation, but a bulging disc is still contained, and a herniation is not.
Pain of Disc Origin
Disc injuries can hurt for many reasons beyond the bulge itself. Research shows that:
The disc can activate nociceptors (pain sensitive nerve fibres) in the outer annulus, ligaments, joint capsules, and nearby muscle structures.
Many large disc bulges or herniations are asymptomatic and may not even be the direct source of pain.
Disc size does NOT reliably predict symptom severity a small bulge can hurt a lot, and a large bulge can hurt very little.
Pain is often worse when the disc is loaded, and relief can occur when it is unloaded or de-loaded.
Inflammation is strongly linked to both pain and disc-degeneration progression, making conservative anti-inflammatory strategies essential.
Most disc herniations improve within 4 to12 weeks using conservative care, regardless of herniation size.
Vertebral Endplate-Mediated Pain
Not all disc pain comes from the disc itself.
Inflammation at the vertebral endplates can appear on MRI as Modic Type 1 changes, which are strongly linked to low back pain.
These changes are inflammation-based, not mechanical, and often respond better to conservative care than fatty Modic Type 2 changes.
Newer imaging tools (e.g., UTE MRI and MRS) are showing promise for detecting biochemical pain generators, but for now, we still rely on history plus physical exam, plus MRI referral when needed.
Spinal Manipulation and the Intervertebral Disc
Here’s the clinical reality based on 25 years in practice:
Chiropractors do adjust in disc cases, but within clinical tolerance and when red flags are absent.
Often spinal adjustments can be paired with mechanical decompression, orthopaedic assessment, posture shifts, and rehab protocols to remove the cause of pressure.
In my practice, spinal adjustments are applied gradually and selectively. We don’t “force discs back in,” we reduce load bearing pressure caused by spinal dysfunction around the disc.
Flexion distraction and traction-based approaches do provide measurable symptom reduction by reducing mechanical load on the affected disc.
My clinical rule:
If a patient tolerates movement, position-based unloading, and neuro-orthopaedic testing, and red flags are absent, then chiropractic assessment is safe and appropriate.
If neurological function progressively worsens then escalation is advised.
How Can a Chiropractor Help a Herniated Disc?
At Up Chiropractic in Leederville Perth, disc cases are assessed every week. Most involve middle-aged people getting back into activity and injuring a disc already weakened by degeneration or loading pressure from spinal dysfunction.
We don’t just treat the disc pain, we identify the cause of load and remove it using evidence-consistent care the body can tolerate.
What Is the Difference Between a Bulging Disc and a Herniated Disc?
Bulge: Contained deformation of the annulus.
Herniation: A tear in the annulus allows nucleus material to break through into the canal.
Bulge = contained, herniation = through a tear, pain = treat the pressure not only the picture.
What Causes a Herniated Disc?
Common causes include:
Age-related disc degeneration creating pre-existing weakness in the annulus.
Repetitive micro-trauma from poor posture and bad ergonomics.
Sudden trauma falls, accidents, or heavy lifting with rotation.
Lifestyle factors: smoking, obesity, sedentary work, lack of exercise.
Poor lifting mechanics.
Clinical Example:
A patient bends, lifts, and twists awkwardly carrying exercise equipment. The disc was already dehydrated and load-intolerant, and the sudden pressure caused a rupture of the annulus. The object being lifted, doesn’t need to be heavy. The worse case that I have seen, a patient was simply picking up an empty milk crate, meaning the problem pre dated the injury.
What Are the Symptoms of a Herniated Disc?
Symptoms depend on both severity and location.
Cervical (Neck) Disc Herniation
May include:
Sharp, shooting pain into upper back, shoulder blades, arms, hands, or fingers
Numbness or tingling
Muscle weakness
Consistent neck pain and discomfort
Red flag: altered gait, Hoffman sign, or symptoms of myelopathy = urgent referral consideration
Lumbar (Lower Back) Disc Herniation
May include:
Sharp or radiating pain into low back, glutes, legs, or feet
Tingling or numbness
Muscle weakness
Persistent low back pain
Red flag: saddle numbness or bladder/bowel dysfunction (possible cauda equina) = seek urgent medical care
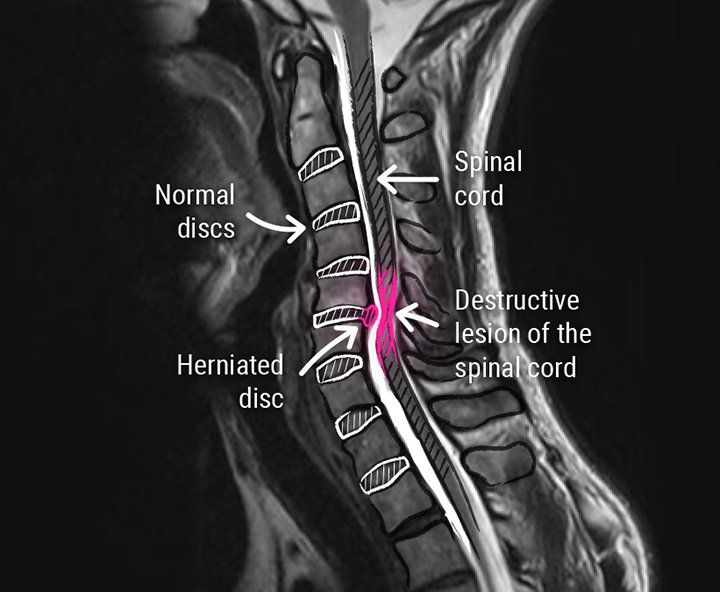
How Is a Herniated Disc Diagnosed?
Diagnosis is based on:
Thorough medical history
Orthopaedic testing
Neurological examination
Functional movement assessment
Referral for MRI only if symptoms fail to improve with conservative care
In my practice we assess load bearing changes using erect, weight-bearing spinal X-rays to map pressure points in posture and movement.
What Activities Should You Avoid With a Herniated Disc?
Avoid movements that dramatically increase intradiscal pressure:
Heavy lifting beyond tolerance
Repetitive bending, twisting, or rotations
High-impact running or jumping if symptomatic
Lifting with rotation
Clinical insight: I don’t tell people to stop moving, I tell them to stop loading it wrong.
Safe & Effective Exercise for Herniated Discs
Great rehab options include:
Spinal decompression / traction positions
Extension-based unloading if tolerated
Modified Child’s Pose
Core motor control rehab
De-loading movements to reduce nerve pressure
Always stop if the movement increases symptoms.
Resolution of the Herniated Disc
Most patients improve in 6 to12 weeks if inflammation calms and load is reduced.
In practice, I have seen many patients:
Avoid surgery
Report major radicular pain reduction
Return to walking, sleep, and sitting tolerance
And in multiple cases, MRI scans show measurable reduction in disc bulge size after conservative chiropractic-led care.
Key clinical reality:
A disc may get smaller, dehydrated, resorbed, or unchanged, but pain and disability often still improve. Size alone is not the recovery story.
What I Want Every Patient to Know
Disc pain is serious, but not always surgical
Most improve if load is removed and neurology calms
Chiropractic care treats the cause of pressure, not only the label
The body needs safety, movement, support, and time, not fear
Get Back to Living Pain-Free
A bulging or herniated disc is not a life sentence. What matters most is that you restore:
✔ Movement
✔ Function
✔ Stability
✔ Load tolerance
✔ Neurological calm
✔ Smarter posture and lifting habits
When we treat in that order, patients recover well.
Conclusion: Should You See a Chiropractor?
Yes! At Up Chiropractic, Leederville Perth, our Chiropractor’s assess you properly, use ortho-neuro exams, and performs spinal adjustments within patient tolerance and without red flags.
Chiropractic care works best when it:
Removes disc-loading forces from spinal dysfunction
Improves neurology and pain response
Restores movement capacity
Supports a favourable natural inflammatory recovery timeline
It is not about cracking a joint, it is about reducing load at the cause so the disc and nerve can breathe, move, and recover.
How can we help?
If you’re experiencing disc-related back or nerve pain in Perth or Leederville, a Chiropractic assessment can give you clarity, direction, and a tailored non-surgical path forward.
At Up Chiropractic, Leederville Perth, we assess discs clinically, treat gently within tolerance, remove the cause of pressure, restore function, and set a rehab plan that helps you avoid recurrence and recover faster.
Book your consultation if you’re:
Hurting in the desk chair but relieved by off-load positions
Experiencing nerve pain, tingling, or weakness
Or unsure if the disc is the true source
Smarter assessment. Safer spine. Better recovery.
1. Saal JA, Saal JS. Natural history and nonoperative treatment of lumbar disc herniation. Spine. 1996;21(24):2904–2911.
🔗 https://pubmed.ncbi.nlm.nih.gov/9112320/ PubMed
2. Schoenfeld AJ, et al. “Treatment of lumbar disc herniation: Evidence-based practice.” PMC Article. 2010.
🔗 https://pmc.ncbi.nlm.nih.gov/articles/PMC2915533/ PMC
3. Gupta A, Upadhyaya S, Yeung C, et al. Does size matter? An analysis of the effect of lumbar disc herniation size on the success of nonoperative treatment. Global Spine Journal. 2020;10(7):881–887.
🔗 https://pubmed.ncbi.nlm.nih.gov/32905720/ PubMed+1
4. Nguyen C, Poiraudeau S, Rannou F. From Modic 1 vertebral-endplate subchondral bone signal changes detected by MRI to the concept of ‘active discopathy’. Ann Rheum Dis. 2015;74(8):1488–94.
🔗 https://pubmed.ncbi.nlm.nih.gov/25977562/ PubMed+1
5. Boisson M, et al. Active discopathy: a clinical reality. RMD Open. 2018.
🔗 https://rmdopen.bmj.com/content/4/1/e000660 rmdopen.bmj.com
6. Splendiani A, et al. Modic I changes size increase from supine to standing MRI correlates with increased pain intensity in standing — biomechanical stress and ‘active discopathy’. Eur Spine J. 2019.
🔗 https://link.springer.com/article/10.1007/s00586-019-05974-7 SpringerLink
7. Orthopaedic Reviews – open medical publishing. Prevalence, clinical predictors and mechanisms of resorption in lumbar disc herniation: a systematic review. 2024.
🔗 https://orthopedicreviews.openmedicalpublishing.org/article/121399-prevalence-clinical-predictors-and-mechanisms-of-resorption-in-lumbar-disc-herniation-a-systematic-review orthopedicreviews.openmedicalpublishing.org
8. Kakhki MK, et al. Effective Conservative Treatments for Lumbar Disc Herniation: Short-Term Reabsorption Through Rehabilitation Techniques. 2025.
🔗 https://www.scivisionpub.com/pdfs/effective-conservative-treatments-for-lumbar-disc-herniation-a-study-on-short-term-reabsorption-through-rehabilitation-techniques-4072.pdf scivisionpub.com